Anemia During Cancer
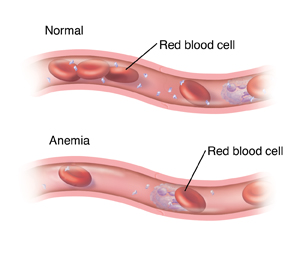
Anemia is when the number of healthy red blood cells (RBCs) in the body drops below normal. It's a very common blood problem. It's often linked to things like blood loss, low iron, or vitamin and mineral deficiency.
Cancer and cancer treatments often cause anemia. Read on to learn more about anemia during cancer and how it’s treated.
What is anemia?
RBCs are made in the bone marrow. Bone marrow is the soft, fatty tissue inside the center of bones. RBCs carry oxygen to the cells in the body. If you have low levels of RBCs, not enough oxygen is sent to your body tissues. This can cause symptoms like:
-
Feeling dizzy or weak.
-
Extreme tiredness (fatigue).
-
Trouble doing daily tasks.
-
Feeling cold all the time.
-
Pale skin, nails, mouth, and gums.
-
Shortness of breath that may be worse with activity.
-
Fast heartbeat.
-
Chest pain.
But some people with anemia have no symptoms. This can be the case if anemia slowly occurs over a long time.
Talk with your doctor if you have any symptoms of anemia. There are many ways to treat it and help keep it from getting worse.
How is anemia diagnosed?
Blood tests are used to look for anemia. A complete blood count (CBC) test is done during cancer care and treatment to measure the number of red blood cells in the blood. One of the things it also measures is your hemoglobin level. Hemoglobin is the iron-rich part of red blood cells that carries oxygen.
Many people with cancer have anemia. Blood tests can help figure out the cause. Then it can be treated, if needed.
Why anemia can happen with cancer
Anemia during cancer can have many causes. These include:
-
Treatments that harm bone marrow. These include some chemotherapy medicines and radiation therapy.
-
Cancer reduces iron use in the body. This is due to the inflammation that cancer causes.
-
Some types of cancer that cause blood loss. This includes lung, ovary, stomach, and colon cancers.
-
Cancer that affects bone marrow function. This includes leukemia, lymphoma, and myeloma.
-
Blood loss during surgery. Losing a lot of blood during cancer surgery can cause anemia.
-
Low levels of some vitamins and minerals. Not enough B vitamins, folate (folic acid), or iron in your blood can cause anemia.
-
Kidney disease. This can lead to low levels of the hormone erythropoietin (EPO). The body needs this to make RBCs.
-
Nausea, vomiting, and appetite loss. These can lead to nutritional problems and weight loss. This lowers the body’s ability to make RBCs.
Treating anemia during cancer
Treatment for anemia depends on what's causing it. It also depends on your symptoms and how bad they are. Your doctor can tell you more about your treatment options and their risks and benefits for you.
Treatment is used to increase your hemoglobin level and ease symptoms caused by anemia. It can include:
-
RBC transfusion. RBCs from a donor can be added to your blood through an IV (intravenous) line that's put into a vein. For a short time, this increases the number of healthy RBCs in your body. A blood transfusion can reverse anemia very quickly. Transfusions are generally safe. Still, there are some risks. Your doctor will discuss them with you before treatment.
-
Erythropoiesis-stimulating agent (ESA). These medicines cause the body to make more RBCs. An ESA is given as a shot. It may be given along with iron (see below). An ESA takes many weeks or even months to slowly improve anemia. There are some risks with ESA medicines. Your doctor will talk with you about them. Be sure you understand these risks.
-
Iron treatments. Some people can take iron pills. Or a liquid iron medicine may be put into your blood in an IV line. Several treatments may be given. IV iron might be used if you're given an ESA. IV iron usually takes a month or so to reverse anemia.
-
Other supplements. You may take vitamin B or folate supplements. These are taken by mouth as a liquid or pill. Oral supplements can take a few months to improve anemia. Be sure you know how and when to take them. Some vitamins may be given as a shot (injection), like vitamin B-12.
-
Diet changes. Eating more foods that are high in iron, folate, and B vitamins may help with a deficiency. Foods high in iron include red meat, poultry, spinach, kale, beans, lentils, tofu, and fortified cereals. Ask your doctor for a list of iron-rich foods.
Checking your progress
During and after treatment, you’ll have many blood tests done. These are to watch your blood cell levels. They check your response to treatment.
Risks and possible complications
Each treatment for anemia has its own risks. Your doctor will tell you what to watch for based on the treatment used. These may include:
Tell your doctor about any side effects you have.